What is the Prostate?
The prostate is a soft gland about the size of a ping-pong ball. It is located below the bladder and in front of the rectum. The prostate is divided into several anatomical regions, or zones. Most prostate cancers begin in the peripheral zone, which is located on the back side of the prostate, near the rectum. For this reason, this part of the prostate can be easily felt during a digital rectal exam. For this reason, examining the prostate with a digital rectal exam is considered a useful screening test.
İçerik
- What is the Prostate?
- What is Prostate Cancer?
- Symptoms of prostate cancer
- How is Prostate Cancer Diagnosed?
- What is a Prostate a Biopsy?
- What is Prostate Fusion Biopsy?
- What are the advantages of fusion biopsy?
- What is Perineal Fusion Biopsy?
- What Are the Advantages of Perineal Fusion Biopsy?
- Stages of Prostate Cancer
- Prostat Kanseri Tedavisi
- Treatment Options for Advanced (Metastatic) Prostate Cancer
- Quality of Life After Prostate Cancer Treatment
- Lifestyle Changes
- FREQUENTLY ASKED QUESTIONS ABOUT PROSTATE CANCER
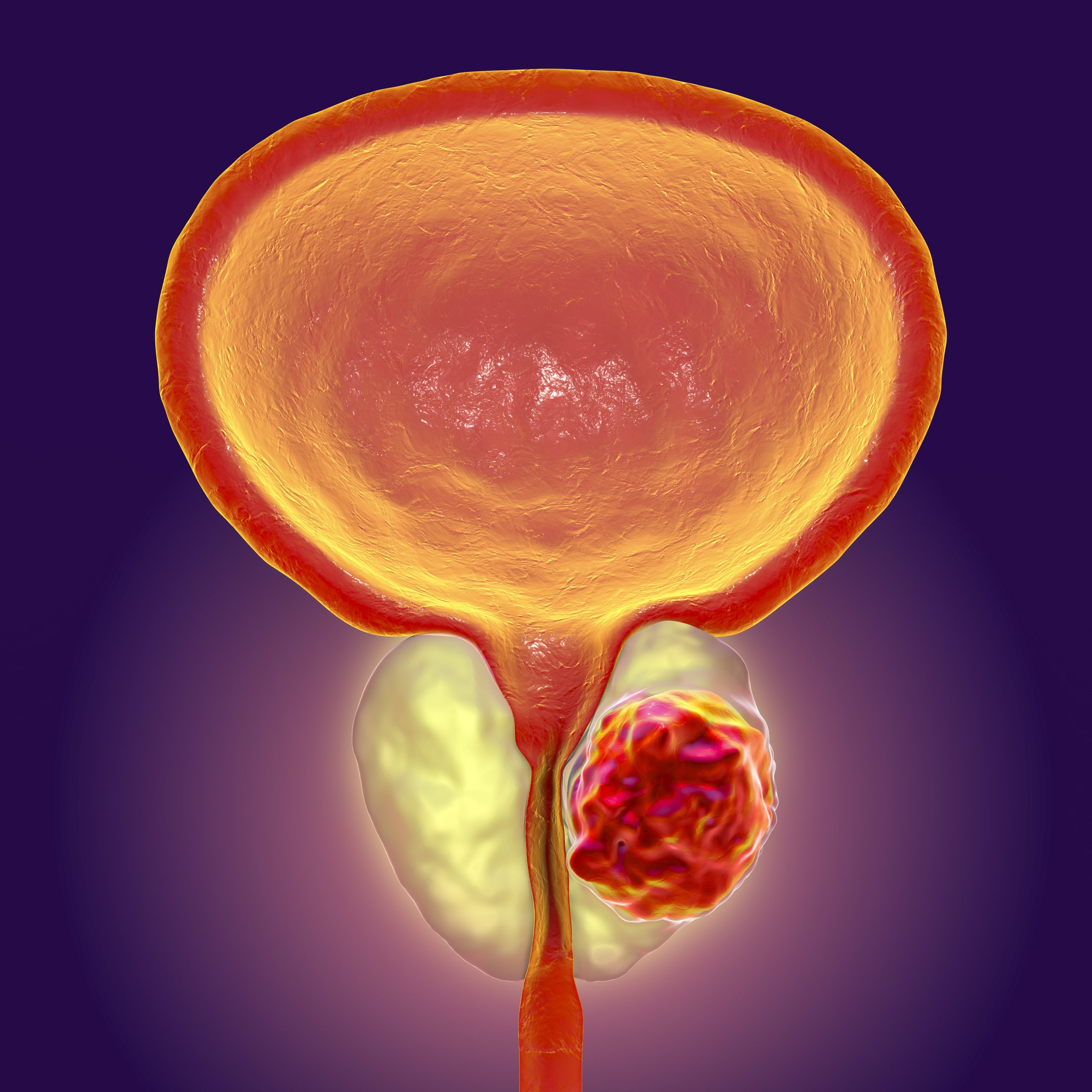
What is Prostate Cancer?
To properly understand the diagnosis and treatment options for prostate cancer, it is important to know how the cancer grows. A normal prostate uses androgens (such as testosterone and dihydrotestosterone - DHT) during its development and daily functions.
Once prostate cancer develops, these cancer cells continue to use androgens as fuel for growth. Therefore, one of the cornerstones of treatment for advanced prostate cancer is hormone therapy, which aims to reduce androgen levels.
- Androgens: Hormones that are important for the functions of the male reproductive system and the development of certain male characteristics.
- Grade: A measure of how abnormal prostate cancer cells appear under a microscope. It is used to estimate how quickly the cancer may grow or spread.
The growth and spread of prostate cancer are directly related to the grade of the cancer cells. This is assessed using the Gleason score system or the ISUP (International Society of Urological Pathology) classification system .
- Gleason Score: This indicates how different the cancer cells are from normal cells. A score of 6 is considered low risk, 7 is moderate risk, and 8-10 is high risk.
- The ISUP Classification is a system used to determine the risk of prostate cancer, rated on a scale from 1 to 5; 1 represents the lowest risk, and 5 represents the highest risk level.
Don't delay, let's meet now !
- Feneryolu Bagdat Avenue No 85/1 Postal Code: 34724 Kadıköy/İstanbul - Turkey
Symptoms of prostate cancer
Prostate cancer often does not cause any symptoms in its early stages.
Prostate cancer may not cause any symptoms in the early stages until the tumor presses on surrounding organs, such as the bladder, urethra, or rectum. In advanced cases, or in patients with metastasis, symptoms may include widespread bone pain, back pain, weight loss, nausea, vomiting, and loss of appetite.
Common symptoms:
- Frequent urination, especially at night
- Urgent need to urinate
- Difficulty starting to urinate
- Difficulty urinating and prolonged urination
- Decreased urine flow
- Feeling that the bladder is not completely empty
- Blood in urine or semen ( )
- In advanced cases, bone pain, back pain, weight loss, nausea, vomiting, and loss of appetite
How is Prostate Cancer Diagnosed?
Prostate cancer can be detected with a PSA (Prostate Specific Antigen) test and a digital rectal exam (DRE) even when there are no symptoms. These methods allow the disease to be detected in its early stages, which increases the success of treatment and reduces side effects.
- Digital Rectal Exam (DRE): The doctor inserts a finger into the rectum using lubricating vaseline and checks the size, shape, and firmness of the prostate.
- PSA Test: A blood sample is taken from your arm, regardless of whether you are fasting or not, to measure your PSA level. A PSA level below 3.0 ng/mL is generally considered "normal." However, the following factors should also be taken into account for a normal evaluation:
- The patient's age
- The size of the prostate
- Previous PSA test results
- Other medical conditions (such as BPH or prostatitis)
- Medications that can lower PSA levels (e.g., Finasteride or Dutasteride)
- Urinary tract infections or procedures
- Multiparametric prostate MRI: Identifies suspicious tumor areas within the prostate, assigns a risk score to these areas, and provides a roadmap for tissue sampling during fusion biopsy.
Diagnosis through biopsy
Although elevated PSA levels may lead a doctor to suspect prostate cancer, the PSA test alone does not provide a definitive diagnosis. The PSA test serves as an early warning system to determine whether further testing is necessary. A prostate biopsy is typically performed.
What is a Prostate a Biopsy?
- The only way to detect prostate cancer, the most common type of cancer in men, is to take a biopsy from the prostate.
- In cases where prostate cancer is suspected based on examination, laboratory tests, and imaging methods, a prostate biopsy must be performed.
- Prostate biopsy can be performed in two ways: classic and fusion biopsy.
- In the traditional method, under local anesthesia and guided by ultrasound, 12 samples are taken from specific areas of the prostate using a special needle ( ).
What is Prostate Fusion Biopsy?
- In prostate fusion biopsy, the areas suspected of cancer in the prostate, as identified in the previously obtained MRI, are determined, and the fusion of these areas with the ultrasound image—that is, overlaying and combining them—is performed immediately before the procedure.
- In fusion biopsy, tissue samples are taken from these suspicious areas under anesthesia and direct visualization, targeting the specific areas.
- The procedure takes approximately 20-30 minutes and does not require hospitalization.
What are the advantages of fusion biopsy?
- The most important advantage is that it can detect clinically significant prostate cancer more effectively than the traditional method.
- Fusion biopsy is typically performed under anesthesia, with the patient sedated. As a result, the patient does not experience any discomfort or pain during the procedure. In contrast, traditional biopsy is often performed under local anesthesia.
What is Perineal Fusion Biopsy?
- Prostate fusion biopsy can be performed using two methods: transrectal and perineal.
- In the transrectal method, the biopsy needle is inserted through the rectum to obtain tissue samples from the prostate, while in the perineal method, the needle is inserted through the perineal region, which is the skin area immediately above the anal region, to obtain tissue samples.
What Are the Advantages of Perineal Fusion Biopsy?
- The risk of infection and sepsis, the most significant complication associated with prostate biopsy, is approximately 10 times lower with the perineal method.
- Sampling of tumor foci in the anterior part of the prostate that cannot be reached by the transrectal method is performed more effectively.
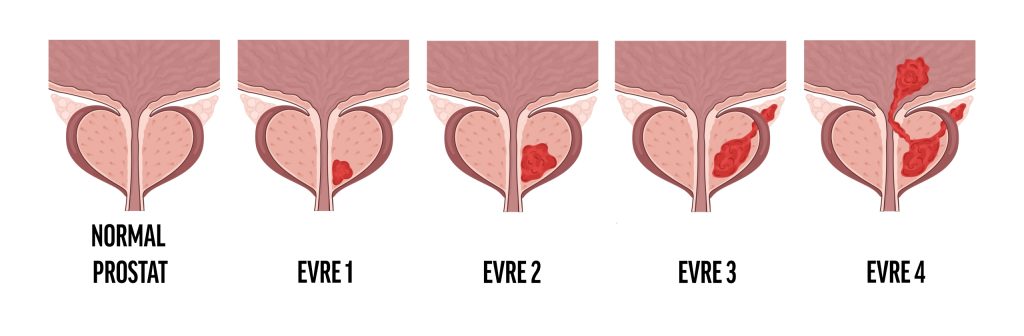
Stages of Prostate Cancer
The stage of prostate cancer indicates the extent of the cancer's spread and plays a critical role in determining the treatment plan.
Staging is based on four main components:
1. PSA Level:
-
- Measured through a blood test, and your doctor will review the most recent values.
2. Grade:
Tissue samples obtained through a biopsy are examined under a microscope by a pathologist, who assigns a grade.
Gleason Score: A classic scoring system. A score ranging from 6 to 10 is assigned. (6 low risk, 7 moderate risk, 8-10 high risk)
ISUP Classification: Revised by the World Health Organization in 2014. Rated from 1 to 5.
| ISUP Grade Grubu | Gleason Score |
|---|---|
| 1 (Low) | ≤ 6 |
| 2 (Moderate - Favorable) | 7 (3+4) |
| 3 (Moderate-Unfavorable) | 7 (4+3) |
| 4 (High) | 8 |
| 5 (Very High) | 9–10 |
3.Tumor Staging (T-Stage):
- T1: Tumor detected by biopsy ( ) performed on suspicion not identified by physical examination or imaging ( ) ( ).
- T2: Nodules detectable during digital rectal examination.
- T3: Tumor extending beyond the prostate capsule.
- T3a: Extending beyond the capsule but not into the seminal vesicles.
- T3b: Tumor that has spread to the seminal vesicles.
- T4: Advanced tumor with invasion into the rectum or bladder.
4.Metastasis Status (N and M Stages):
- N (Lymph Node): Indicates whether cancer is present in the lymph nodes.
- M (Metastasis): Indicates whether the cancer has spread to bones or other organs.
- Imaging is recommended in high-risk patients (PSA >20, Gleason 8-10, T3 or T4 stage).
Prostat Kanseri Tedavisi
How is Prostate Cancer Treated?
Treatment Selection:
There is no standard treatment for prostate cancer; each patient requires a personalized treatment plan. In some cases, your doctor may not recommend immediate treatment. This approach is called "watchful waiting" or "active surveillance." Instead of starting treatment, the disease is monitored through regular checkups, and intervention is initiated if the cancer shows signs of progression.
Determining Treatment Options:
Factors to consider when determining your treatment plan include:
- Need for treatment
- Family genetics
- Risk level based on biopsy and examination results
- Personal preferences and lifestyle
- Risks and side effects associated with treatment
Determining the Treatment Option
A man diagnosed with localized (not spread beyond the prostate) or locally advanced (spread to nearby tissues) prostate cancer has three main treatment options:
- Active surveillance
Active surveillance aims to regularly monitor patients with slow-growing prostate cancer without immediate surgery or radiation therapy. The disease is monitored with annual PSA tests, digital rectal exams (DRE), and biopsies if necessary. If the disease progresses, treatment options are evaluated.
Who is eligible for Active Surveillance?
Criteria for Active Surveillance:
- Grade Group 1 (Gleason Score 6),
- PSA <10,
- The cancer is confined to the prostate,
- Very few cancer foci found on biopsy.
Ideal candidate: Young or middle-aged men with low-risk prostate cancer.
- Surgery
Radical Prostatectomy
The complete removal of the prostate gland is called "radical prostatectomy." This treatment method is commonly preferred when prostate cancer has not spread. Additionally, in advanced or recurrent cases, additional surgical procedures such as lymph node removal may be performed.
Surgical Methods:
- Open Radical Prostatectomy
- This is the traditional surgical method.
- An incision is made in the lower abdomen, and the prostate is completely removed.
- Sometimes the prostate can also be removed from the area between the scrotum and the anus (perineal route), but this technique is rarely used.
- Laparoscopic (Robot-Assisted) Radical Prostatectomy:
- This procedure has become popular in the last 10 years.
- Several small incisions are made in the abdominal area.
- The surgeon performs the operation with high precision using robotic arms.
- A camera and surgical instruments are inserted through these small incisions.
- Studies indicate that robotic surgery offers a shorter recovery time compared to open surgery.
Post-Surgery Recovery Process:
- Patients typically stay in the hospital for 2–5 nights after surgery.
- A catheter is typically used at home for 7 to 14 days to facilitate urine flow.
- Urinary incontinence is common in the first weeks and months.
- This usually improves within the first year, but may be permanent for some patients.
- Kegel exercises are recommended to help control urination.
- Avoid physical activities such as heavy lifting and weight training for the first 2 months.
- Radiotherapy
Radiotherapy is sometimes combined with hormone therapy, but surgery is generally not performed in conjunction with hormonal therapy.
- Other Alternative Treatment Options:
In recent years, some new treatment options have emerged:
- Cryotherapy: Aims to destroy cancer cells by freezing them.
- High-Intensity Focused Ultrasound (HIFU): Destroys tumor cells using high-intensity sound waves.
Nanoknife method: This method has begun to be used in the treatment of clinically insignificant, small-volume, low-risk prostate cancers. Also used in some pancreatic and liver tumors, this method is safely applied in the treatment of prostate cancer. In the Nanoknife method, special electrodes are placed around the tumor in the prostate using ultrasound guidance. These electrodes are then sequentially exposed to very high doses of electrical current for short durations. This creates an electromagnetic field in the area, permanently increasing the permeability of cell walls. As a result, tumor cells lose their viability.
Treatment Options for Advanced (Metastatic) Prostate Cancer
What is Advanced Prostate Cancer?
Metastatic prostate cancer is characterized by the spread of cancer cells from the prostate to lymph nodes, bones, or other organs. Prostate cancer often metastasizes to bones first (in 85–90% of cases). However, it can rarely spread to the liver, lungs, or brain.
Primary Hormone Therapy
Prostate cancer cells require androgens such as testosterone to grow. Therefore, hormone therapy is used to reduce testosterone levels in metastatic prostate cancer.
Intermittent Hormone Therapy
In intermittent hormone therapy, hormone suppression therapy is paused at regular intervals and then restarted.
- The goal here is to minimize treatment-related side effects while maintaining efficacy.
- During hormone therapy, PSA levels decrease; after a period of time, treatment is stopped, and when PSA begins to rise again, it is restarted.
Advantages:
- Reduced side effects (e.g., hot flashes, loss of libido).
- Reduced negative effects on bone density.
Disadvantages:
- A consistent response to hormone therapy may not be achieved.
- Some studies have observed that it is not as effective as continuous treatment.
Hormone-Sensitive Prostate Cancer
If the disease has not been previously exposed to hormone therapy, it is defined as "hormone-sensitive." Treatment begins with hormone-suppressing therapies. In recent years, combination therapy approaches using chemotherapy and new-generation hormone therapies have yielded successful results in patients with hormone-sensitive metastatic prostate cancer.
Hormone-Resistant Prostate Cancer
If the cancer continues to progress despite hormone therapy, the disease is classified as "hormone-resistant." In this case, standard hormone therapies are ineffective.
Quality of Life After Prostate Cancer Treatment
Prostate cancer treatment, while helping to control the disease, may also bring about certain side effects and lifestyle changes. The main issues patients may face after treatment include:
Urinary Control
- Urinary Incontinence: Temporary or permanent urinary incontinence may occur after prostatectomy or radiation therapy.
- Stress Incontinence: Urinary leakage during coughing, sneezing, or laughing.
- Urgent Incontinence: A sudden urge to urinate.
Treatment Recommendations:
- Kegel Exercises: Recommended to strengthen the pelvic floor muscles.
- Biofeedback Therapy: Used to learn how to properly contract the muscles.
- Medication: May help control bladder muscles.
- Surgical Options: Artificial urinary sphincters or sling surgeries may be performed in severe cases.
Sexual Function
- Erectile dysfunction is common after surgery and radiation therapy.
- Damage to the neurovascular bundles can affect erectile function.
Treatment Options:
- Oral Medications: Viagra (Sildenafil), Cialis (Tadalafil), Levitra (Vardenafil).
- Injection Therapies: Alprostadil is injected directly into the penis.
- Vacuum Devices: Increase blood flow into the penis.
- Penile Prostheses: Surgical implants that provide a permanent solution.
- Penis Rehabilitation: Programs initiated after treatment to ensure regular blood flow.
Long-Term Effects of Hormone Therapy
Some side effects may be permanent after hormone therapy:
- Muscle loss and weakness
- Bone density loss (osteoporosis)
- Loss of libido and sexual dysfunction
- Risk of diabetes and heart disease
Recommendations:
- Regular exercise programs
- Calcium and vitamin D supplements
- Medications that increase bone density (Zoledronic Acid, Denosumab)
Psychological Support and Mental Health
Psychological effects are commonly seen after prostate cancer treatment:
- Anxiety and depression
- Fear of cancer recurrence after treatment
- Loss of self-confidence due to sexual dysfunction
Support Options:
- Psychological counseling and therapy
- Participation in support groups
- Mindfulness and stress management techniques
Lifestyle Changes
Diet
- Foods high in antioxidants: Tomatoes (lycopene), broccoli, leafy green vegetables.
- Lean proteins: Fish, poultry, legumes.
- High-fiber foods: Whole grains, vegetables, and fruits.
- Avoid sugar and saturated fats: Opt for natural and fresh foods instead of processed foods.
- Exercise and Physical Activity
- At least 150 minutes of moderate exercise per week, such as walking, cycling, or swimming, is recommended.
- Weight-bearing exercises are important for maintaining muscle mass and increasing bone density.
- Regular exercise reduces the risk of depression and increases energy levels.
- Smoking and Alcohol Consumption
- Smoking increases the risk of prostate cancer recurrence; quitting after treatment is strongly recommended.
- Alcohol consumption should be kept to a minimum; heavy drinking should be avoided.

