What Are Testicles and How Do They Work?
Male reproductive organs consist of internal and external parts. The main reproductive organs are the penis, testicles, and prostate gland. The penis and testicles are the external male reproductive organs.
These male reproductive organs are designed to perform the following functions:
- To produce and secrete male hormones for the growth of muscles, bones, and body hair
- Producing and transporting sperm and the fluid (semen) that protects it for reproduction
- Transporting sperm to the female reproductive system
The testicles are two small, egg-shaped glands located in a sac (scrotum) beneath the penis. This is where sperm are produced and mature. Sperm travel from here to the vas deferens (a "tube" behind the testicles) and are expelled through the urethra during ejaculation. The testicles also produce male hormones such as testosterone. Testosterone controls sexual drive in males and initiates the growth of muscles, bones, and body hair.
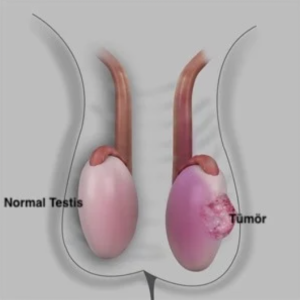
Healthy testicles have a firm and slightly spongy texture. The firmness should be consistent throughout. Both testicles should be approximately the same size, although one may be slightly larger than the other.
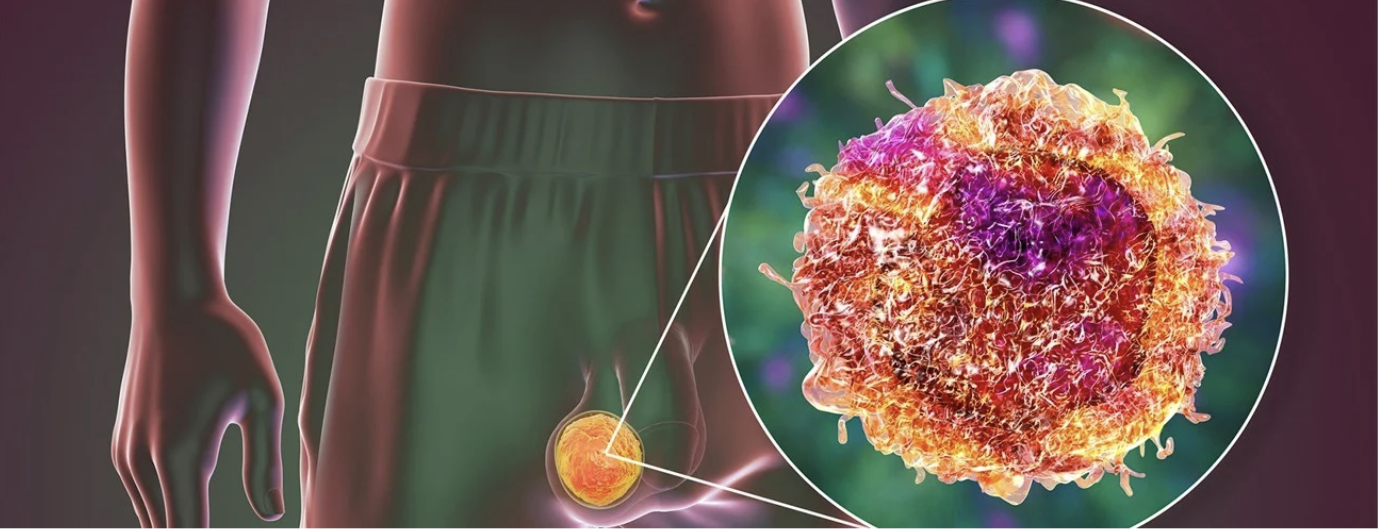
What is Testicular Cancer?
Testicular cancer occurs when cells in the testicle grow and form a tumour. This condition is rare. Over 90 per cent of testicular cancers start in the germ cells that produce sperm. There are two types of germ cell tumours (GCT). Seminoma grows slowly and responds very well to radiation and chemotherapy. Non-seminoma, on the other hand, can grow rapidly.
There are several types of non-seminoma: choriocarcinoma, embryonal carcinoma, teratoma, and yolk sac tumours.
There are also rare types of testicular cancer that do not originate in germ cells, such as Leydig cell tumours and Sertoli cell tumours.
Testicular tumours may also present as tumours composed of multiple cell types.
The type of testicular cancer cell found, symptoms, and other factors will help guide your treatment.
Testicular Cancer Symptoms
The symptoms of testicular cancer can be difficult to detect, especially in the early stages. The symptoms of a testicular tumour include:
- A painless swelling in the testicle, which is the most common symptom
- Painful or painless swelling of the testicle
- A feeling of heaviness in the testicles
- A dull ache or soreness in the testicle, scrotum, or groin
- Sensitivity or changes in male breast tissue
If you feel any lump or hardness in your testicle, you should see a doctor to find out if it is a tumour. You should get tested as soon as possible. Approximately 75 out of 100 men with a lump or swelling in their testicle have cancer. On average, most men do not tell anyone about these symptoms.
If you wait, the cancer may spread. If you notice swelling that lasts longer than two weeks, it is very important to talk to your urologist. The urologist will determine whether the swelling is cancerous. Other conditions that can cause swelling:
- Epididymitis: Swelling of the epididymis. It is usually treated with antibiotics.
- Testicular torsion: twisting of the testicles. This is usually treated with surgery.
- Inguinal hernia: Part of the intestine protruding through a weak spot in the abdominal muscles in the groin area. It is usually treated with surgery.
- Hydrocele: A build-up of fluid in the scrotum. It is not dangerous, but if it causes discomfort, it can be treated surgically.
What causes testicular cancer?
It is not always known why cells grow to form tumours. Furthermore, you may not be able to avoid the risk factors for testicular cancer. The best plan is to diagnose the problem early.
Don't delay, let's meet now !
- Feneryolu Bagdat Avenue No 85/1 Postal Code: 34724 Kadıköy/İstanbul - Turkey
Who Gets Testicular Cancer?
Although the exact cause of testicular cancer is unknown, certain risk factors increase the likelihood of developing the disease:
The risk of testicular cancer increases in men with the following conditions:
- Family history: If your father or brother has had testicular cancer.
- Undescended testicles: If your testicles did not descend before birth. This condition may also be referred to as cryptorchidism and is when the testicle has not descended from the abdominal area into the scrotum as it should have before birth. The likelihood of a tumour developing is higher after this problem. The testicle can be brought down through surgical intervention, but cancer may still develop.
- GCNIS: These are unusual cells called germ cell neoplasia in situ (GCNIS) in the testicle and are usually found during infertility testing.
Microlithiasis, or small calcifications in the testicle, is not a risk factor for testicular cancer, but it can be considered a risk factor when combined with the risk factors listed above.
Testicular Cancer Diagnosis
Many men can detect whether there is a problem with their testicles by performing a self-examination. Testicular cancer is one of the most treatable types of cancer. When diagnosed early, the cure rate is approximately 100 per cent. This applies to men with early-stage testicular cancer that has not spread beyond the testicle. Even in men with stage II or III testicular cancer, the cure rate is still higher than for other types of cancer. If you notice a lump in your testicles or scrotum, or if you experience discomfort, pain, or other changes, you should definitely see a urologist.
Don't delay, let's meet now !
- Feneryolu Bagdat Avenue No 85/1 Postal Code: 34724 Kadıköy/İstanbul - Turkey
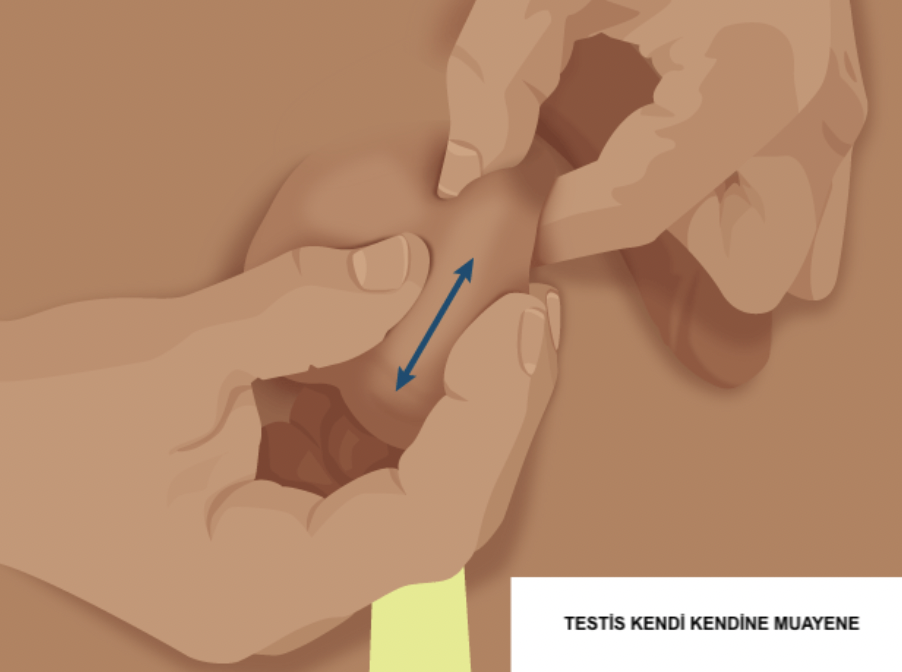
1.Self-Examination of the Testicles
The best time to perform a monthly testicular examination is after a warm bath or shower, while standing, when the scrotum is relaxed. This procedure takes only a few minutes. To begin:
- Check each testicle. Gently but firmly roll each testicle between your thumb and forefinger. Feel the entire surface. The firmness of the testicle should be the same all over. It is normal for one testicle to be slightly larger than the other.
- Check for any swelling, lumps, or anything that does not look normal. Swellings or lumps are not normal (even if they do not cause pain). Pain is not normal.
- Check yourself at least once a month. Always check for changes in size, shape, or texture. If you notice a lump or any change over time, you should seek medical help. It may be nothing serious, but if it is testicular cancer, it can spread very quickly. Testicular cancer is treatable when diagnosed early. If you have any questions or concerns, talk to your urologist.
2. PHYSICAL EXAMINATION
Your urologist will examine your scrotum, abdomen, lymph nodes and other areas for signs of cancer. They will check for any signs of swelling, hardness or tenderness. If you have a history of undescended testicles, it is very important to inform your doctor.
3. TESTICULAR ULTRASOUND
This imaging test is used to view the inside of the scrotum and check for any suspicious lumps. If your doctor wants to see inside your chest or abdomen, other scans or X-rays may also be performed. This is done to see if the cancer has spread to the lymph nodes, lungs or liver. MRI is rarely used, but in some cases it is necessary to check the brain and spinal cord.
4. BLOOD TEST
A blood test is performed to check for tumour markers specific to testicular cancer. These are proteins and hormones produced by some types of testicular cancer. AFP, HCG and LDH tumour markers are elevated in some cancers, but some types of testicular cancer do not produce tumour markers. In other words, normal tumour markers do not mean you are cancer-free.
Tumour markers (AFP, HCG, and LDH) must be measured before any treatment, such as surgery. If cancer is detected, tumour marker tests are repeated after treatment to monitor your progress over time. Certain medications and cannabis can cause false positive results in HCG levels. Inform your doctor about any medication and/or cannabis use.
Stages of Testicular Cancer
If your urologist detects cancer as a result of these examinations, they will want to determine the exact type of cancer cell and whether it has spread. This is called staging. This process helps the doctor determine the most appropriate treatment.
Testicular cancer cannot be detected by a standard biopsy (tissue sample). In this type of cancer, the cancerous tissue is removed surgically and the cells are then examined.
Testicular cancer is divided into the following stages:
Stage 0: This stage is also called Germ Cell Neoplasia In Situ (GCNIS). This is not yet cancer, but it is a warning sign that cancer may develop. GCNIS can be found in the seminiferous tubules and nowhere else.
Stage I (IA, IB, IS): The cancer is confined to the testicle. It has not spread to nearby lymph nodes or other parts of the body.
Stage II (IIA, IIB, IIIC): The cancer has spread to one or more lymph nodes in the abdominal area (this is usually the first area to which testicular cancer spreads). It has not spread to other parts of the body.
Stage III (IIIA, IIIB, IIIC): The cancer has spread beyond the lymph nodes in the abdominal area. The cancer may be found in distant lymph nodes or in distant sites such as the lungs. Tumour marker levels are high.

Testicular Cancer Treatment Methods
Treatment for testicular cancer varies depending on the stage and type of tumour. Typically, a team of doctors, including a urologist, oncologist, and radiation oncologist, work together to determine the best treatment plan for each patient. Decisions are made based on the patient's specific diagnosis and overall health.
Before treatment, men should discuss with their urologist whether they wish to have children. Infertility and changes in male hormones are common after some treatments. If you particularly wish to have children in the future, it may be beneficial to consider sperm banking before treatment.
Men can also obtain information about testicular prostheses before surgery. A testicular prosthesis is a way to make the scrotum appear more "normal" after the testicle has been removed.
-
Follow-up:
After the tumour-containing testicle is removed and staging is performed, some patients may be suitable for monitoring without the need for additional treatment. Monitoring is a way to track changes through regular check-ups. These include physical examinations, tumour marker tests, and imaging tests. Low testosterone symptoms can also be monitored in most men.
As described below, surveillance may be recommended for stage 0 and some stage I cancer patients.
Stage I seminoma. Surveillance is an option for stage I seminoma following surgery. It should include physical examination and imaging and should also cover tumour markers.
Stage I non-seminoma germ cell tumours (NSGCT). Surveillance is an option for stage I NSGCT following surgery. It should include physical examination, imaging, and tumour marker testing. If signs of cancer growth are present during surveillance or if there are changes in hormone levels, further treatment may be recommended.
2. Surgery:
- ORCHIDECTOMY
The first-line treatment is the removal of the testicle through the groin (radical orchiectomy). Orchiectomy is used to diagnose and treat early-stage or advanced-stage cancer. In this surgery, the testicle and tumour are completely removed through a small incision made in the groin area. The spermatic cord is also removed. After the surgery, the pathologist stages the cell type.
Patients often ask, "How long does testicular cancer surgery take?" This operation usually takes about 1 hour. Routine follow-up is performed after surgery to ensure that the cancer does not recur. Also, if the patient is concerned about his appearance, a testicular prosthesis (artificial testicle) may be an option.
- TESTICULAR-SAVING SURGERY
Testicular-sparing surgery (TSS) may be recommended for a very limited group of patients. In this procedure, only the tumour tissue is removed, not the entire testicle. For TSS, the mass must be very small and tumour markers must be negative. TSS is a suitable method for men with benign tumours rather than cancer. If the tumour is cancerous and the patient has a normal testicle on the other side, TSS is not recommended.
Follow-up is important after surgery to monitor for cancer.
- RETROPERITONEAL LYMPH NODE DISSECTION
Retroperitoneal lymph node dissection (RPLND) is a complex surgery that may be beneficial for some men. A skilled surgeon is required to remove the lymph nodes behind the abdomen to ensure that side effects are kept to a minimum. This surgery is an option for patients with more aggressive Stage I cancer. It is generally used in men with non-seminomatous germ cell tumours that are likely to recur. It may be used instead of chemotherapy in Stage IIA or IIB non-seminoma tumours. Following RPLND surgery, chemotherapy or surveillance may be recommended depending on the location, type, and risk of recurrence of the cancer.
3. Chemotherapy:
It is preferred especially in non-seminomas and advanced-stage disease.
4. Radiotherapy:
Primarily used in seminomas.
Treatment-Related Risks:
Patients who have undergone radiation and/or chemotherapy should pay attention to their heart health. The risk of cardiovascular disease increases after treatment. Simple lifestyle changes can prevent problems. For example, try to exercise regularly, consume less processed foods, and quit smoking/vaping. Do not forget to have regular check-ups to monitor your blood pressure, lipid and glucose levels.
Patients who have undergone radiation and/or chemotherapy may have a higher risk of developing different types of cancer in the future.
Men who have undergone testicular cancer treatment may also have lower testosterone levels. Patients should be monitored for signs and symptoms of low testosterone and, if symptoms arise, should be checked with a blood test.
Risk of Recurrence After Treatment:
The risk of testicular cancer recurrence depends on the stage at diagnosis. The risk of cancer developing in the other testicle is also higher than in normal individuals. In this regard, learning how to perform self-examination of the testicles is very important. It is also crucial not to neglect regular follow-ups with your urologist.
If the cancer reappears, your doctor will want to detect it and treat it quickly. Additional treatment depends on the type and location of the cancer. Options include RPLND surgery, radiation and chemotherapy.
Sexual Life and Fertility After Treatment
Removal of one testicle should not significantly affect your sexual energy or fertility (your chances of having children) if the other testicle is normal. Most men can achieve normal erections after surgery. However, men diagnosed with testicular cancer have a higher risk of infertility and low testosterone. Chemotherapy or radiation therapy may cause a decrease in sperm count, but this usually resolves. If lymph nodes have been removed, ejaculation may become difficult. If you experience problems, there are treatments available to help with ejaculation.
As you recover, your body will find its balance. Over time, the healthy testicle will usually produce enough testosterone to help you return to normal. Your doctor may check your hormone levels annually as part of your check-up.
